RIP IVF? NHS cuts to fertility treatment ‘will deny thousands parenthood’
Exclusive: Some areas that once offered couples three cycles of IVF may soon provide none
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Couples struggling to have children are increasingly likely to be denied NHS-funded fertility treatment, with several Clinical Commissioning Groups preparing to halt or restrict offering IVF because of financial concerns.
Mid and North East Essex became the first CCGs in the country to stop funding treatment for healthy couples last month, and more are now planning to do the same.
The Basildon and Brentwood group, also in Essex, and South Norfolk are considering slashing funding from three and two IVF cycles per couple respectively to zero. Somerset CCG has proposed to reduce funding from two cycles to one with decisions expected by January.
The groups have all cited funding pressures as the reason behind the proposed changes, and the simultaneous timing has sparked concerns that more CCGs may follow suit.
The two Essex CCGs will only fund treatment in “exceptional circumstances” – for example where the male partner has a transmittable infection or one partner is undergoing cancer treatment.
The National Institute for Health and Care Excellence (Nice) recommends up to three cycles of IVF for women under 40 who have not conceived after two years and one cycle for some women aged between 40 and 42.
One IVF cycle results in a live birth for just under 33 per cent of women aged 35 or younger, 28 per cent of women aged 36-37 and 21 per cent of women aged 38-39, and just over one in eight women aged 40-42 will be successful. Having just one cycle therefore severely limits the chances of couples having children.
However, new figures published on 2 November by campaign group Fertility Fairness show that just one in five CCGs provide three cycles – a drop of 6 per cent since 2013 – with fewer than one in four offering two cycles.
The number of CCGs offering only one cycle has risen to 57 per cent – exacerbating the “postcode lottery” in fertility treatment as more couples are priced out of parenthood. One IVF cycle at a private clinic costs around £5,000.
Concerns over the future of IVF funding in England come at the start of National Fertility Awareness week which aims to provide extra help for the one in six couples who struggle to become parents.
Fertility Fairness has written to Health minister Jane Ellison requesting a meeting to discuss the “urgent and worrying trend in IVF provision in England”.
Co-chairs Susan Seenan and Sarah Norcross said in their letter: “IVF has long been subject to a postcode lottery but some good progress was made over the last Parliament, and at the end of 2014 every CCG in England was funding at least one cycle of IVF for the first time.
“However, we are now witnessing a reversal of this trend… We would like to see definite action to prevent this decommissioning becoming an automatic policy change for CCGs seeking to make financial savings.”

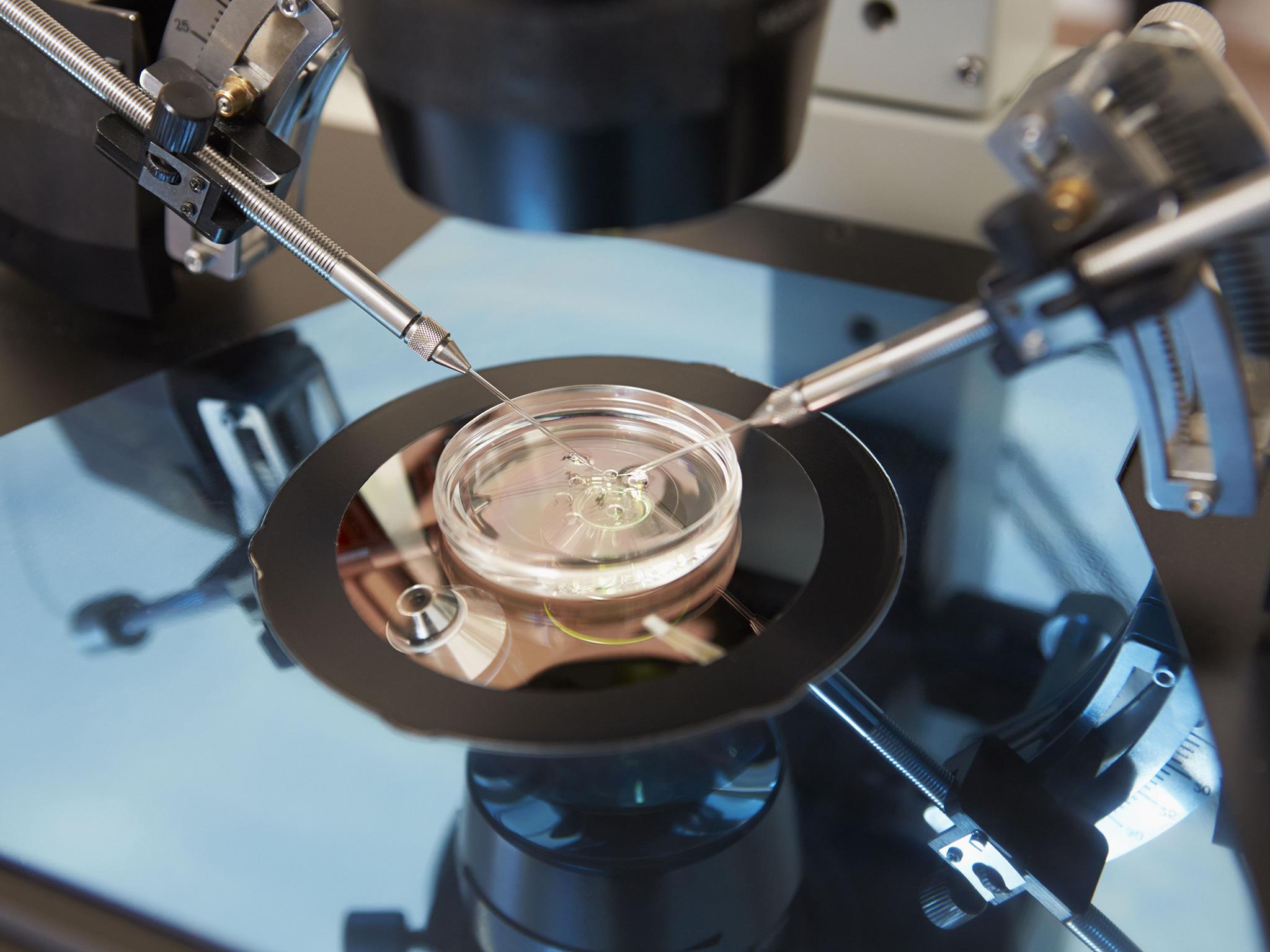
One woman from Essex who was recently turned down for NHS funding told The Independent of her disgust. She and her husband have been trying to conceive for more than a year and were hoping to be referred by their GP to a clinic for intra-cytoplasmic sperm injection (ICSI) – a type of IVF treatment that involves the injection of a single sperm directly into each egg.
“We were told that although our doctor would refer us for funding, it was highly unlikely we would be funded due to being in the mid-Essex CCG,” said the 28-year-old, who did not want to be identified.
“This is a huge blow.Although we are not low earners we will struggle to come up with the £6,000 to £7,000 we would need for ICSI and would definitely not be able to afford more than one cycle.
“Knowing we won’t get help adds to the heartache we are feeling. I understand funds need to be cut but to remove all funding is disgusting.”
Ms Seenan said the Essex CCGs’ decision to stop funding was deeply worrying. “They’ve gone from a very good provision to nothing,” she said. “We are concerned that there’s a possibility more CCGs may follow. It’s completely wrong of them not to be adhering to Nice guidance.”
Fertility Fairness is calling for the Nice guidelines to be mandatory and for greater collaboration between CCGs so they can provide more treatment without impacting on their budgets. The 24 CCGs that make up the North and North West collaboratives all provide three IVF cycles.
The luck of the draw depends on where a patient’s GP surgery is located – not where they live. CCGs also differ over eligibility criteria meaning if a man has children from a previous relationship, IVF treatment might be denied his current partner regardless of her situation.
“The complicated and varied criteria is also blatantly unfair,” Ms Seenan said. “Patients just can’t understand it.”
Dr Amanda Doyle, a GP who is co-chair of NHS Clinical Commissioners, said: “CCGs are led by GPs whose first priority is always to the patient and where possible we want to give them what they need, including fertility treatment.
“Unfortunately, the NHS does not have unlimited resources and ensuring patients get the best possible care against a backdrop of squeezed finances is one of the biggest issues CCGs face. As a result there are some tough choices that have to made.”
Doing damage: Male fertility risks
Many men are unaware that getting older, drinking too much and being obese can reduce their fertility, according to a new poll. Almost half (49 per cent) of more than 2,000 men polled by Nuffield Health, in partnership with the charity Infertility Network UK, were not aware that sperm suffers more genetic faults as men get older. More than one in three men were unaware that drinking alcohol reduced fertility.

Learning by mistakes: IVF is trial and error
Sarah Davies-Smith gave birth two years ago to twin girls, Rosie and Lily, following her third round of IVF. But her local CCG, Bedfordshire, recently altered its policy from offering three cycles to just one.
We just wouldn’t be parents had we not had the third and final attempt,” she said.
“It just seems unfair that other people are going to be put through this all over the country. It takes a while for clinics to work out the best method for you, the right amount and different kinds of drugs, and what might have gone wrong.
“It took two failed attempts in my case and if we hadn’t had the third we are not in a position to afford IVF privately to pay the thousands of pounds each time that it costs.”
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments