Cancer treatment using nanotechnology tested with 'astounding' results
Scientists believe technique could offer treatment for metastatic cancer of lungs and liver after successful tests on mice

Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.A new cancer treatment that uses nanotechnology has shown “astounding” results in mice.
Scientists believe the technique could offer a treatment for metastatic cancer of the lungs and liver, two of the main causes of death for patients with a wide range of incurable cancers that have spread around the body.
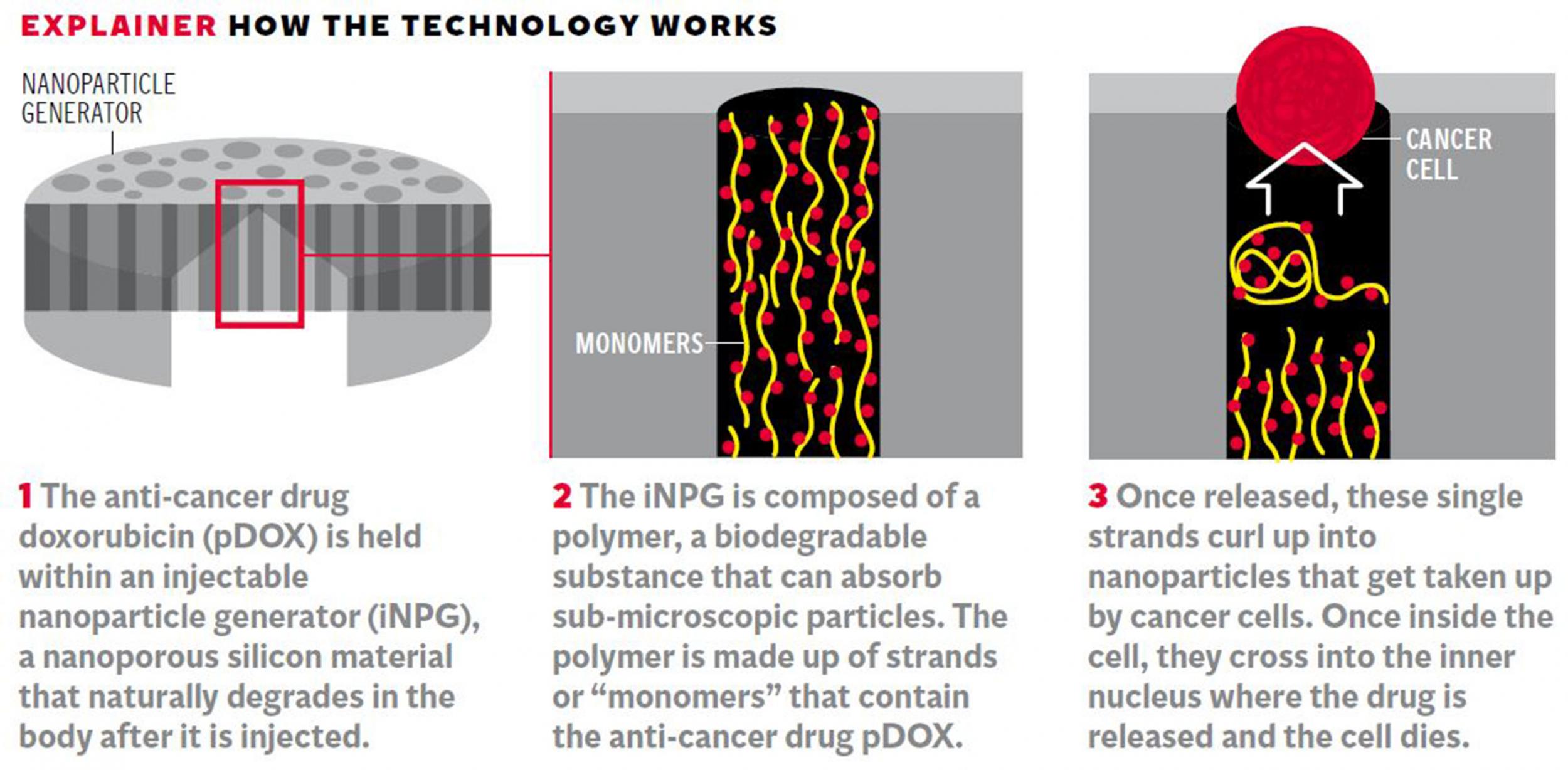
The researchers developed a method of delivering anti-cancer drugs to these vital organs using a “nanoparticle generator” that can bypass a tumour cell’s ability to develop drug resistance.
Tests on mice with incurable breast cancer that has spread to the lungs shows that half of them were effectively cured of the disease after eight months of follow-up – equivalent to 24 years of long-term survival in humans.
If the finding were to be replicated by other researchers, it would represent a new milestone in cancer therapy, coming just weeks after breakthroughs in cancer immunology where the body’s own immune defences were shown to be capable of launching an attack on spreading tumours.
The latest treatment is based on injecting the patient with a porous silicon material that has been absorbed with an anti-cancer drug. After injection into the blood stream, the material is carried to the site of a tumour where the silicon breaks down to produce cancer-killing nanoparticles.
Click HERE for larger annotated version of the graphic
Mauro Ferrari, the scientist who led the work at the Houston Methodist Research Institute in Texas, said that the results on mice are unprecedented and clinical trials on the first human patients could begin as early as next year, using a “nanoparticle generator” to improve the potency of existing anti-cancer drugs.
“To my very best understanding, this is the first case we’ve ever seen of a therapy with a well understood mechanism that can provide long-term, disease-free survival of our pre-clinical animal populations,” Dr Ferrari said.
“If this bears out in the clinical realm, even a short fraction in the preclinical experimentation that we did, it will be transformational. It will be the first ever demonstration of a cure of metastatic disease to the lungs,” he said.
The study, published in the journal Nature Biotechnology, used a standard chemotherapy drug called doxorubicin. However, it was the drug-delivery mechanism, using nanotechnology, that produced the stunning results, he said. Nanotechnology refers to the science of extremely small things, and the approach has recently seen major breakthroughs in an array of scientific fields.
“Lung and liver metastases are the two main reasons why we lose cancer patients. The results we have proven with this paper is that we can provide a functional cure; we can essentially cure long-term, [giving] disease-free survival for about 50 per cent of the animals that we provided this therapy to,” Dr Ferrari said.
“Through understanding the mechanism we can begin to think about strategies that will work for the other 50 per cent as well,” he said.
“If this research bears out in humans and we see even a fraction of this survival time, we are still talking about dramatically extending life for many years. That’s essentially providing a cure in a patient population that is now being told there is none,” he added.
The nanoparticle generator effectively concentrates the anti-cancer drug within the tumour cells, leaving healthy cells untouched, which should avoid many of the toxic side-effect seen in patients treated conventionally. The nanoparticle polymer breaks down into single strands that curl up into nanoparticles. These are quickly absorbed by cancer cells and taken into the cell nucleus where the drug is released and the cell dies.

“This may sound like science fiction, like we’ve penetrated and destroyed the Death Star, but what we discovered is transformational. We invented a method that actually makes the nanoparticles inside the cancer and release the drug particles at the site of the cellular nucleus,” Dr Ferrari said.
“I would never want to overpromise to the thousands of cancer patients looking for a cure, but the data is astounding. We’re talking about changing the landscape of curing metastatic disease, so it’s no longer a death sentence,” he said.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments