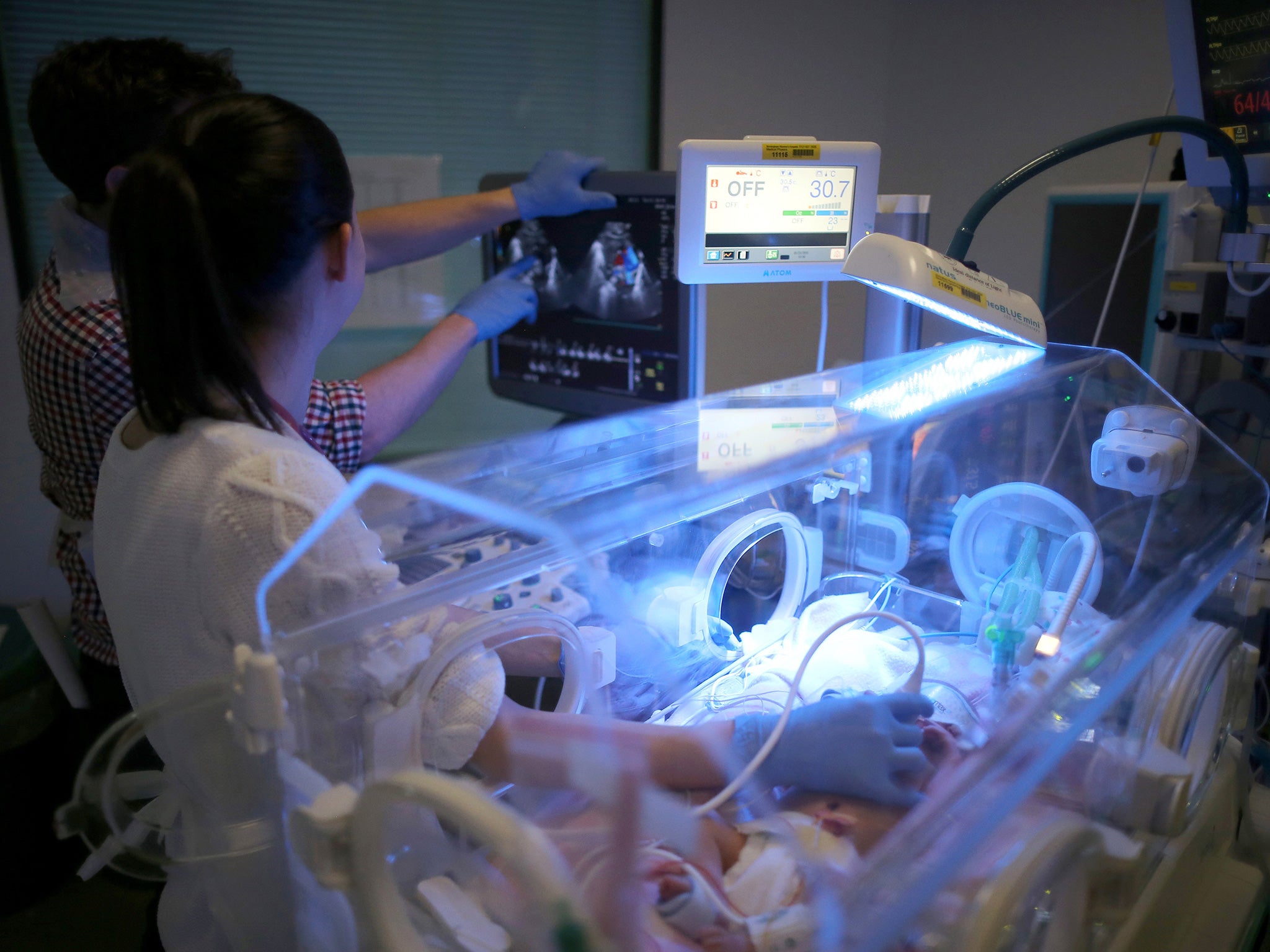
Analysis of infant deaths finds UK could save the lives of up to 2,000 babies a year
Newborns' survival rates in Britain compare unfavourably with Europe's best

Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.The lives of up to 2,000 babies could be saved every year if the UK could match the best survival rates in Europe, a new analysis of stillbirths and new-born deaths has found.
While survival rates have improved, six in every 1,000 babies born in the UK is stillborn or dies soon after birth. This compares to 4.3 in every 1,000 in Sweden.
Researchers also found that mortality rates were significantly higher at some NHS hospitals than others, ranging from 5.4 deaths per 1,000 births in the best-performing NHS area to 7.1 per 1,000 in the worst-performing – suggesting that hundreds of lives could be saved if the worst hospitals performed as well as the best.
Overall, there were 3,286 stillbirths in the UK in 2013, and 1,436 deaths in the first four weeks after birth, from a total of 781,929 births, according to the MBRRACE-UK report, compiled by a team of academics, clinicians and charities.
The differences in mortality rates between hospitals were observed even when factors known to affect infant mortality rates, such as poverty levels in the patient population, were taken into account. The names of the best and worst-performing NHS providers and commissioners will be released on Wednesday.
Professor David Field, a neonatal specialist at the University of Leicester, who co-authored the report said that parts of the UK with the highest number of baby deaths should be subject to “thorough reviews” of their maternity and neonatal care.
The report also found that babies born to mothers living in poorer areas, as well as those born to black and Asian mothers, were more likely to die.
Stillbirth or neonatal death was 50 per cent more likely in areas with the highest levels of poverty, and babies of black or black British, and Asian or Asian British ethnicity had the highest mortality rates, of 9.8 and 8.8 deaths per 1,000 deaths.
The authors of the report said that hospitals and NHS commissioners should set “national aspirational targets” for stillbirth and neonatal mortality rates.
Co-author Professor Elizabeth Draper, also of the University of Leicester, said the report confirmed the UK performs “poorly compared to other European countries of similar economic status” and urged the NHS to set “benchmarks” to help hospitals improve.
A national review of NHS maternity services in England is currently underway. Launched in the wake of a report into failings at Morecambe Bay NHS Foundation Trust, which led to the preventable deaths of 11 babies, the review, chaired by Baroness Cumberlege, is due to report by the end of the year with recommendations for improving safety of care during pregnancy and at birth.
Professor Neena Modi, president of the Royal College of Paediatrics and Child Health, said the figures represented 15 families “devastated by the death of their baby” every day, while the Royal College of Midwives (RCM) said the report highlighted “real inequalities” for women and babies.
Both groups called for better prevention of lifestyle factors that can lead to problems in pregnancy, including smoking and obesity.
Louise Silverton, director of midwifery at the RCM, that said while NHS could improve, “hard pressed maternity staff can only do so much.”
“Tackling issues like smoking and obesity need political will and intervention at the highest levels,” she said. “There are some real lessons for the Government here, and more must be done to reduce poverty and social exclusion. Both are things which lie at the heart of many of these problems.”
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments