The simple cholesterol test that says if you need statins — and why doctors in UK aren’t using it
Lives are being put at risk, it is claimed, as with current methods of gauging artery-clogging, medics are missing a trick

Your support helps us to tell the story
This election is still a dead heat, according to most polls. In a fight with such wafer-thin margins, we need reporters on the ground talking to the people Trump and Harris are courting. Your support allows us to keep sending journalists to the story.
The Independent is trusted by 27 million Americans from across the entire political spectrum every month. Unlike many other quality news outlets, we choose not to lock you out of our reporting and analysis with paywalls. But quality journalism must still be paid for.
Help us keep bring these critical stories to light. Your support makes all the difference.
Heart disease stubbornly remains one of the biggest killers in the UK, where there are 7 million people living with the condition. During the past 60 years, the management of cholesterol has become an important weapon in the fight against this – and drugs called statins are often used in treatment.
But as a new review highlights, statins can often cause crippling side-effects – and may actually result in more harm than good. Writing in the British Journal of Sports Medicine, Australian science reporter Maryanne Demasi claims that doctors and patients are being misled about the true benefits and harms of these drugs. She also suggests that raw data on their efficacy and safety are being kept secret and have not been subjected to scrutiny by other scientists.
But despite concerns about patients taking them unnecessarily, the use of statins is so widespread that they are now the most prescribed drug in the UK. There have even been recent calls for all males aged over 65 and females over 75 to be prescribed them. If this were to happen it would mean they were used by almost 12 million people across the country.
One of the key diagnostic tests to decide if a person should be put on statins is often a blood cholesterol test. If the results show raised levels, the patient will generally be thought of as being at an increased risk of cardiovascular disease and prescribed statins. But there is mounting evidence which shows this test alone is insufficient in its predictive power.
Cholesterol explained
To make sense of this it helps to understand how cholesterol is transported around our bodies. A simple analogy may be to think of how boats move cargo around waterways. But rather than rivers and canals, our bodies have a network of arteries and capillaries, with “lipoprotein” particles which act like minuscule vessels, constantly shuttling cholesterol back and forth.
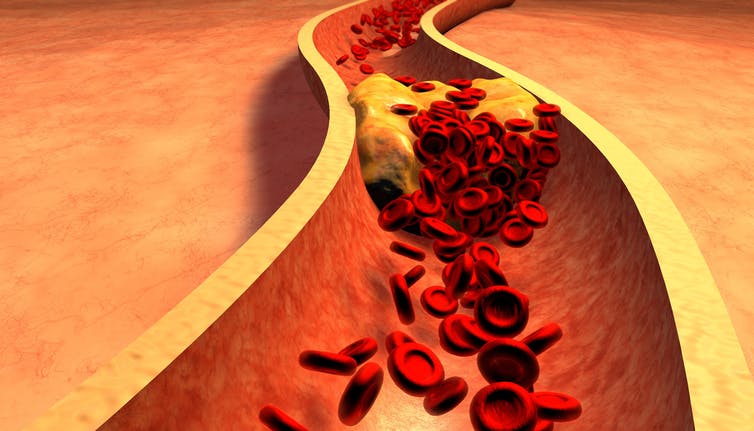
These particles exist in a variety of distinct types, with perhaps the most well known being low-density lipoproteins (LDL) and high-density lipoproteins (HDL). LDL particles are commonly referred to as “bad cholesterol” as they ship cholesterol to the arterial wall where it can potentially form a plaque. Whereas HDL is often known as “good cholesterol” as it removes cholesterol from arteries.
Despite these simplistic explanations it is important to realise that when doctors test for LDL they are actually observing the amount of cholesterol stored on board the boat (or particle), rather than looking at the actual vessel itself. This seemingly minor detail is where problems can arise.
Although conventional wisdom holds that there is a positive relationship between the cholesterol on board LDL particles and cardiovascular risk, we have known for some time through large-scale studies that this is not always the case.
In reality some people with high LDL cholesterol may actually be at a low risk of heart disease and are therefore potentially treated unnecessarily. And in the same way, some individuals with low LDL cholesterol levels can be at an extremely high risk – yet remain untreated due to a lack of diagnosis. The number of people who fall into these categories is substantial – studies suggest up to 20 per cent may be affected.
To address these issues, doctors have now been told to use “non-HDL” cholesterol as a determinant of cardiovascular risk. This encompasses all cholesterol stored in lipoproteins which contribute towards cardiovascular disease, except for HDL.
But although this has been shown to be a better predictor, problems remain. This is mainly because non-HDL is also determined from the cholesterol content of particles, rather than by measuring the particles themselves.
The test
Returning to our earlier analogy, if an enemy armada was approaching at sea, surely it would be better to gauge the threat by counting the number of boats, rather than trying to determine the amount of cargo contained on board. Remarkably, we can do something similar with our lipoproteins.
Attached to each LDL particle is a single molecule of a protein called apolipoprotein B100 (ApoB). And by determining how much ApoB is in the blood we can “count” exactly how many LDL particles are present.
Determining LDL in this way is better than measuring the cholesterol stored inside, because ApoB has been shown to be a superior predictor of cardiovascular disease than measuring both LDL cholesterol and non-HDL cholesterol.
But despite this, tests for ApoB aren’t routinely used – partly because of the cost. An ApoB test is more expensive than using non-HDL alone – which can be quickly and cheaply calculated using data derived from routine lipid checks.
Many doctors may also be simply unaware of the importance of ApoB – despite countries such as Canada incorporating ApoB testing into their guidelines. The UK, for example, has been reluctant to make such recommendations. All of which further perpetuates the hesitance of healthcare professionals to incorporate the measure into their assessments.
But this is highly shortsighted, given the scale of the burden that cardiovascular disease places upon the NHS – and the mass prescription of statins and their widely documented side-effects.
Perhaps then, it is time to ask if the current diagnostic method for blood cholesterol really is the best option.
Richard Webb is a postdoctoral researcher in nutritional science at Liverpool John Moores University. This article was originally published on The Conversation (www.theconversation.com)
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments