Scientists shocked to find antibiotics alleviate symptoms of schizophrenia
Chance discovery of link between acne drug and psychosis may unlock secrets of mental illness
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.A cheap antibiotic normally prescribed to teenagers for acne is to be tested as a treatment to alleviate the symptoms of psychosis in patients with schizophrenia, in a trial that could advance scientific understanding of the causes of mental illness.
The National Institute for Health Research is funding a £1.9m trial of minocycline, which will begin recruiting patients in the UK next month. The research follows case reports from Japan in which the drug was prescribed to patients with schizophrenia who had infections and led to dramatic improvements in their psychotic symptoms.
The chance observation caused researchers to test the drug in patients with schizophrenia around the world. Trials in Israel, Pakistan and Brazil have shown significant improvement in patients treated with the drug.
Scientists believe that schizophrenia and other mental illnesses including depression and Alzheimer's disease may result from inflammatory processes in the brain. Minocycline has anti-inflammatory and neuroprotective effects which they believe could account for the positive findings.
Details of the trial were presented to the independent Schizophrenia Commission by Bill Deakin, professor of psychiatry at the University of Manchester, who is the lead investigator. The 12-member commission, set up by the mental health charity Rethink, is looking into the treatment and care of people with schizophrenia, and is due to report in the summer.
The first account of minocycline's effects appeared in 2007 when a 23-year-old Japanese man was admitted to hospital suffering from persecutory delusions and paranoid ideas. He had no previous psychiatric history but became agitated and suffered auditory hallucinations, anxiety and insomnia.
Blood tests and brain scans showed no abnormality and he was started on the powerful anti-psychotic drug halperidol. The treatment had no effect and he was still suffering from psychotic symptoms a week later when he developed severe pneumonia.
He was prescribed minocycline to treat the pneumonia and within two weeks the infection was cleared and the psychosis resolved. Minocycline was stopped and his psychiatric symptoms worsened. Treatment with the drug was resumed and within three days he was better again. Halperidol was reduced but he remained on minocycline. Two years after his psychotic episode, he was still well.
The UK trial aims to recruit 175 patients recently diagnosed with schizophrenia, half of whom will be randomly allocated to take minocycline with their standard anti-psychotic treatment while the remainder take a placebo.
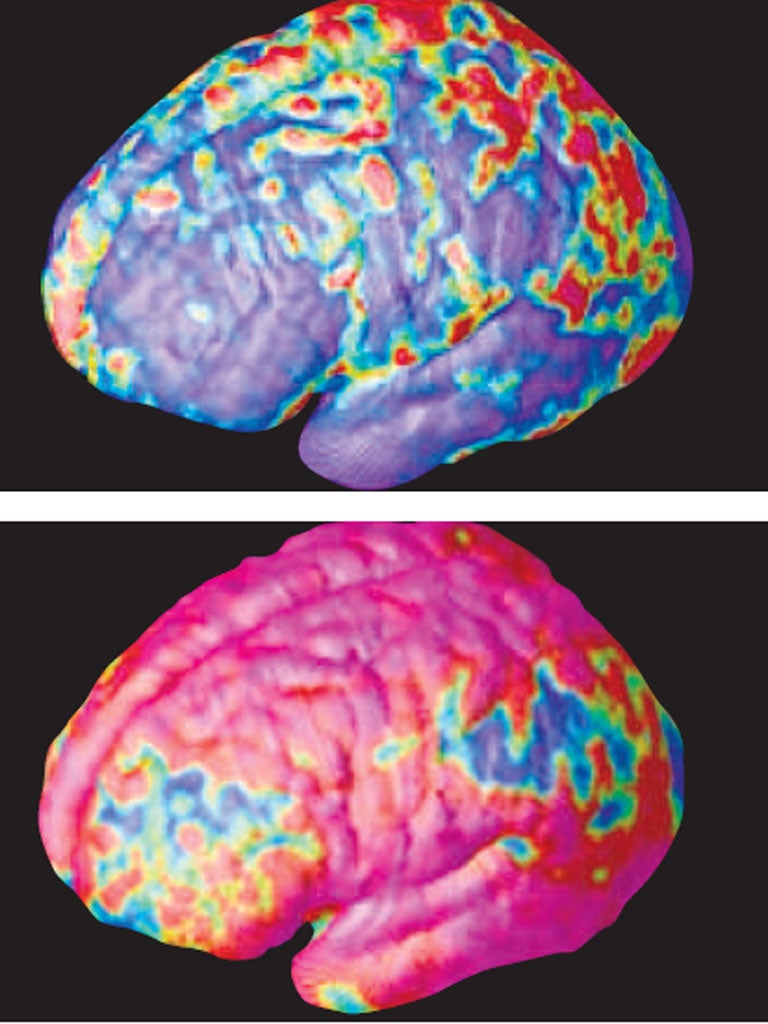
Brain scans will be carried out at the start and end of the 12 month trial to compare loss of grey matter – an effect of schizophrenia – in the two groups. Tests will also measure inflammatory markers in the blood.
Professor Sir Robin Murray, chair of the Schizophrenia Commission said: "Infection or inflammation might be involved in a minority of people with acute psychosis and minocycline might counter this. In depression inflammatory markers go up and in Alzheimer's too."
Jeremy Laurance is a member of the Schizophrenia Commission
Subscribe to Independent Premium to bookmark this article
Want to bookmark your favourite articles and stories to read or reference later? Start your Independent Premium subscription today.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments