Midwife shortage linked to rise in Caesarean births
Warning comes as health body revises guidelines to allow women to demand surgical delivery
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Caesarean birth rates may rise from their present record levels unless urgent action is taken to address the "massive" midwife shortage, childbirth experts have warned.
The warning came as the National Institute for Clinical Excellence (Nice) updated its guidance to enable women to demand a Caesarean section, even when it was not medically necessary and despite its higher cost to the NHS.
The move is intended to help medical staff to intervene earlier with women who may be worried about natural childbirth. Evidence shows most can be reassured about the safety of a vaginal delivery. But if, after discussion of the risks and benefits, a woman still wants a Caesarean, they should be able to have one, the guidance says.
The previous guide, in 2004, said "maternal request is not on its own an indication for Caesarean section" and could be declined by a doctor.
Experts launching the guidance yesterday said they expected demand for Caesareans to fall as a result of earlier intervention and new advice that those who have had two or more Caesareans, and those with HIV, may safely opt for a vaginal birth.
However, a report from the Royal College of Midwives yesterday said the maternity services faced a "looming crisis" as a result of a 22 per cent rise in the birth rate since 2001 and a shortfall of almost 5,000 midwives in England. Lack of midwife support during birth was an important reason for high Caesarean rates, Malcolm Griffiths, consultant obstetrician at Luton and Dunstable Hospital and chairman of the Nice guideline group, said.
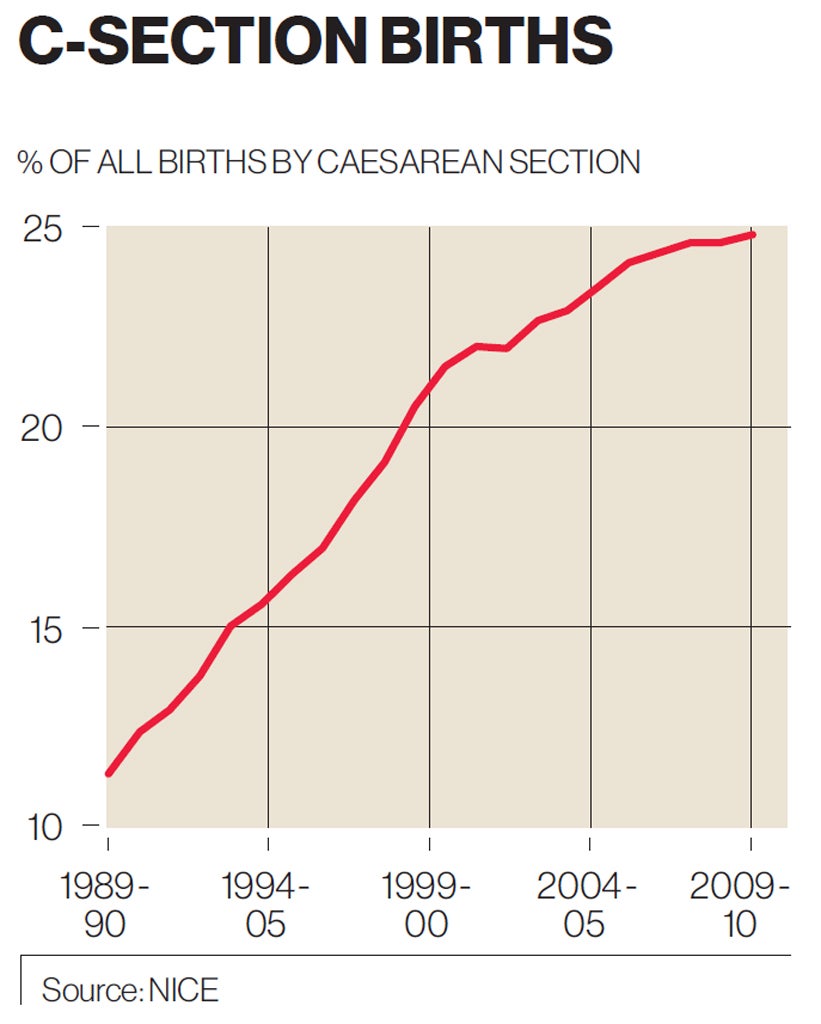
Caesareans have more than doubled in the past 20 years and now account for one in four births in England. The rate varies from 15 to 34 per cent across NHS trusts, and in Europe from 14 per cent in the Nordic countries to 40 per cent in Italy. "The difference is support during labour. That is key to reducing the Caesarean rate. I think the shortage of midwives is a factor [in England's Caesarean rate]," Mr Griffiths said.
Belinda Phipps, chief executive of the National Childbirth Trust, the charity for parents, said: "When women are treated with respect, and are offered support and information tailored to their concerns, very few of them will choose a Caesarean birth unless there are clear health reasons."
A planned Caesarean costs £2,369, and a vaginal birth £1,665, according to Nice. Mr Griffiths said: "Caesarean section is a major operation – about as major as a hysterectomy from which it takes six weeks to recover. Yet we send a woman home two days after a Caesarean and then we say, 'Here's a baby to look after too.' It's not a major operation that most pregnant women are interested in or want to have."
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments